If you want VA disability benefits, you need to be discharged from the military. However, you may be discharged from the military in many different ways – while honorably discharged Veterans can rest assured that they will receive the benefits they need, what about other Veterans with other discharge types?
Today, we’ll break down dishonorable discharge benefits in detail. We’ll also explore the benefits you can expect if you have a discharge type that is something other than honorable or dishonorable.
A dishonorable discharge is only given to Veterans who commit serious crimes during their military service. Dishonorable discharges may only be assigned to Veterans through a court-martial – that usually means that the Veteran in question has to have committed a serious criminal action or otherwise violated the armed forces’ code of conduct.
Unfortunately, many Veterans have received dishonorable discharges because of factors outside their control, such as sexual assault, post-traumatic stress disorder (PTSD), and other similar conditions. Furthermore, a dishonorable discharge makes you ineligible for all VA disability benefits regardless of whether you are injured in the military.
On top of that, your dishonorable discharge determination stays on your military record unless you successfully get the Discharge Review Board to correct or modify it. Such a board can also correct discharge statuses imposed by a court-martial.
Veteran benefits, such as disability compensation or access to the GI Bill, may be denied to dishonorably discharged Veterans.
No. If you are dishonorably discharged for any reason, you are automatically ineligible for VA disability benefits. Even if your injury occurred or was aggravated in the military while performing your duties, you would not be able to turn to the VA for assistance paying for medical and related expenses.
That said, there are some exceptions to dishonorable discharge VA benefits. If you qualify for one or several of these exceptions, you may still qualify for VA disability benefits – especially if you can prove that you qualify to the VA directly.
Qualifying for VA disability benefits can help you overturn or modify a previous dishonorable discharge status. You might be able to overturn your status if you later submit your military record to review by the discharge review board to the Department of Veterans Affairs.
There are two main types of “dishonorable condition” discharges:
Generally speaking, the statutory bar to compensation also prohibits access to VA health care, while the regulatory bar does not. Thus, a Veteran may be barred from receiving compensation benefits but not VA health care.
Statutorily defined dishonorable conditions include:
Regulatorily defined dishonorable conditions include:
The strongest exception regarding benefits is when the Veteran has more than one duty period. For example, suppose the Veteran has a good period of service for VA compensation purposes and a bad period of service. In that case, any disabilities that arose during the good service period are eligible for compensation.
As for exceptions to the “willful misconduct” and “moral turpitude” regulations, minor offenses are not considered willful misconduct if the Veteran’s service was otherwise honest, faithful, and meritorious.
A mere technical violation of police regulation or ordinances does not constitute willful misconduct. Also, VA regulations state that moral turpitude “generally” includes a felony conviction. If the Veteran’s service is generally good, with no felony convictions, they may be entitled to benefits. Therefore, a Veteran may still be eligible for VA benefits.
Entry-level separation administrative discharges do not prohibit a Veteran from receiving benefits. However, a voided enlistment or induction may be a bar to benefits. An exception to this is the termination of active duty service solely on a person’s misrepresentation of their age.
Insanity is another exception to VA rules and regulations. Suppose the VA establishes that the Veteran was insane at the time of the offense leading to the discharge. In that case, the Veteran is not barred from benefits based on their character of discharge determination.
The insanity does not have to be a cause of the misconduct. It is worth noting that the VA’s definition of insanity is broader than the definition used in the criminal defense context.
A Veteran may also be barred from benefits if the cause or aggravator of the disability arose when the Veteran was AWOL. However, it is not enough for the VA to bar benefits just because a Veteran was AWOL.
The VA also must decide whether the Veteran’s absence materially interfered with the performance of military duties. The decision is likely incorrect if the VA denies dishonorable discharge VA benefits without making this determination. This allows the Veteran to appeal the VA’s decision.
Evidence showing that absence may not have interfered with military duties may include:
However, periods of AWOL that exceed 180 continuous days, absent compelling circumstances to warrant the prolonged unauthorized absence, will result in your benefits being denied.
As for discharges accepted in exchange for the military’s promise not to try the Veteran in a court-martial, the bar only applies if the trial was a general court-martial. The law does not say that a threat with a trial by special court-martial would inhibit the Veteran from receiving benefits.
If the record is unclear as to whether the court-martial would be general or special, the Veteran may be able to argue that the benefit of the doubt is in his favor.
A presidential pardon for a court-martial conviction allows the VA to consider the conduct that led to the conviction when determining eligibility for dishonorable discharge VA benefits.
If the Veteran is a victim of military sexual trauma (MST), the VA must provide free care for all physical and mental health conditions related to the trauma. This entitlement to free care from a VA medical center should apply regardless of the characterization of the Veteran’s service.
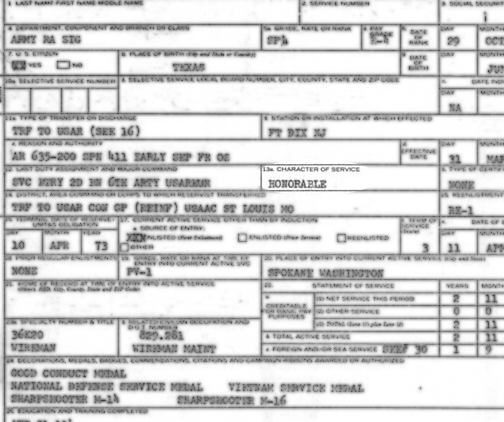
Veterans who receive an honorable discharge status automatically get access to all VA disability benefits, as do dependents, such as spouses or children. However, there are other discharge types.
You may wish to know whether you qualify for VA benefits if you have a discharge status of something other than honorable.
A general discharge is awarded to Veterans who perform to the minimum standards necessary for adequate military work. In essence, a general discharge means that a servicemember met various standards of adequacy but did not perform to such a point as to meet the standards for an honorable discharge.
Some Veterans may qualify for a general discharge under honorable conditions – this indicates that the Veteran generally performed adequately but some difficulty prevented an honorable discharge.
In any case, Veterans with a general discharge status qualify for all VA benefits, including student loan benefits, disability benefits, etc. Furthermore, their dependents, such as spouses and children, should also qualify for VA benefits.
Note that you may receive a general discharge status even if you have some disciplinary marks, but these are usually quite minor.
An other than honorable (OTH) discharge is a type of undesirable discharge. Sometimes called a “bad paper,” an other than honorable discharge is awarded to Veterans who are discharged under middling statuses and reviews.
An other than honorable discharge is a kind of administrative discharge, meaning that it isn’t assigned to a Veteran by a court-martial. If you receive an other than honorable discharge, you should qualify for most VA benefits, including VA disability benefits. However, you may not qualify for other disability benefits, such as certain funeral benefits or student loan benefits.
A bad conduct discharge or BC discharge is a so-called punitive discharge. That means you were discharged under some sort of discipline or punishment. Many servicemembers who receive a bad conduct discharge are barred from reenlistment in the military, and they may be required to serve time in the military prison.
Bad conduct discharges may only be awarded through special courts-martial and criminal trials. You generally do not qualify for VA benefits if you receive a bad conduct discharge. The VA has discretion when deciding whether conduct discharged Veterans will receive disability and other benefits, as the VA is technically a separate organization from the military itself.
Suppose you believe you qualify for one of the above exceptions to a general discharge. In that case, you could get your military record corrected and ensure that you qualify for VA benefits, including disability benefits.
However, you can only do this if you contact knowledgeable Veterans law attorneys. The right Veterans law attorneys can help you appeal or apply for a discharge upgrade through the discharge review board or DRB. The discharge review process through this organization is completely separate from the VA.
Therefore, if your discharge status is upgraded through the DRB, the VA has a license to consider that discharge status upgrade but is not required to automatically start awarding you benefits. Your next step is to appeal directly to the VA itself.
In this appeal process, you will present the evidence of the exception to your dishonorable discharge and evidence that the discharge review board successfully upgraded your discharge status. Combined with relevant medical documents and other information, it’s possible to convince the VA to upgrade your benefits or qualify you for them.
If this occurs, however, note that it will take time. The VA will likely go through this process over several months. The right Veterans law attorneys can help streamline this timeline and help you get the benefits you need as quickly as possible.
A dishonorable discharge isn’t the only circumstance in which you might be denied VA benefits.
For example, the VA does not pay benefits to Veterans who are absent without leave or AWOL for at least 180 days. There is an exception to this, specifically if the VA finds proof that compelling circumstances might excuse the absence.
If you were discharged above the dishonorable level, you still need to apply for your benefits individually. Merely receiving an honorable discharge, for instance, does not mean the VA will start paying your medical bills immediately.
Instead, you’ll need to go through the lengthy benefits claims process with attorneys helping you step-by-step.
Suppose the VA or the discharge review board does not agree that your dishonorable discharge status qualifies under an exception. In that case, you may need financial assistance for your medical bills or disability expenses elsewhere.
Unfortunately, the discharge review board is not perfect, nor is the VA. These organizations can and do make mistakes. If you believe that the VA should upgrade your discharge status or that you should qualify for VA benefits, don’t give up. Veterans law attorneys can help you keep up the fight and pursue a brighter future.
Ultimately, dishonorably discharged Veterans may not receive VA disability benefits unless they qualify for one of the above exceptions. If you believe your dishonorable discharge status should qualify, you may need legal assistance to overturn your discharge status and prove your claim to the VA.
Berry Law can help. Our knowledgeable Veterans law attorneys are well-equipped and ready to assist you and help you ensure you get the benefits you need to secure financial stability for you and your family. Contact us today to learn more.
Sources:
Types of discharge | Vet Verify
CLAIMS FOR VA BENEFITS AND CHARACTER OF DISCHARGE – GENERAL INFORMATION | VA.gov
Applying for Benefits and Your Character of Discharge | VA.gov
Our monthly newsletter features about important and up-to-date veterans' law news, keeping you informed about the changes that matter.